Understanding the problem
Through conversations and workshops, I explored the daily challenges nurses and clinicians faced in intensive care. These conversations revealed the strain of continuous bedside presence, the risk of missing critical changes, and operational bottlenecks.
Defining phase
I mapped out pain points, different flows and journey maps to identify key moments and responsibilities. This research surfaced some critical insights that shaped the product strategy:
No control mechanisms for nurses' unavailability
No overviews Nurses lacked patient status visibility.
Trust issues with new tech, AI, workflows and reliability
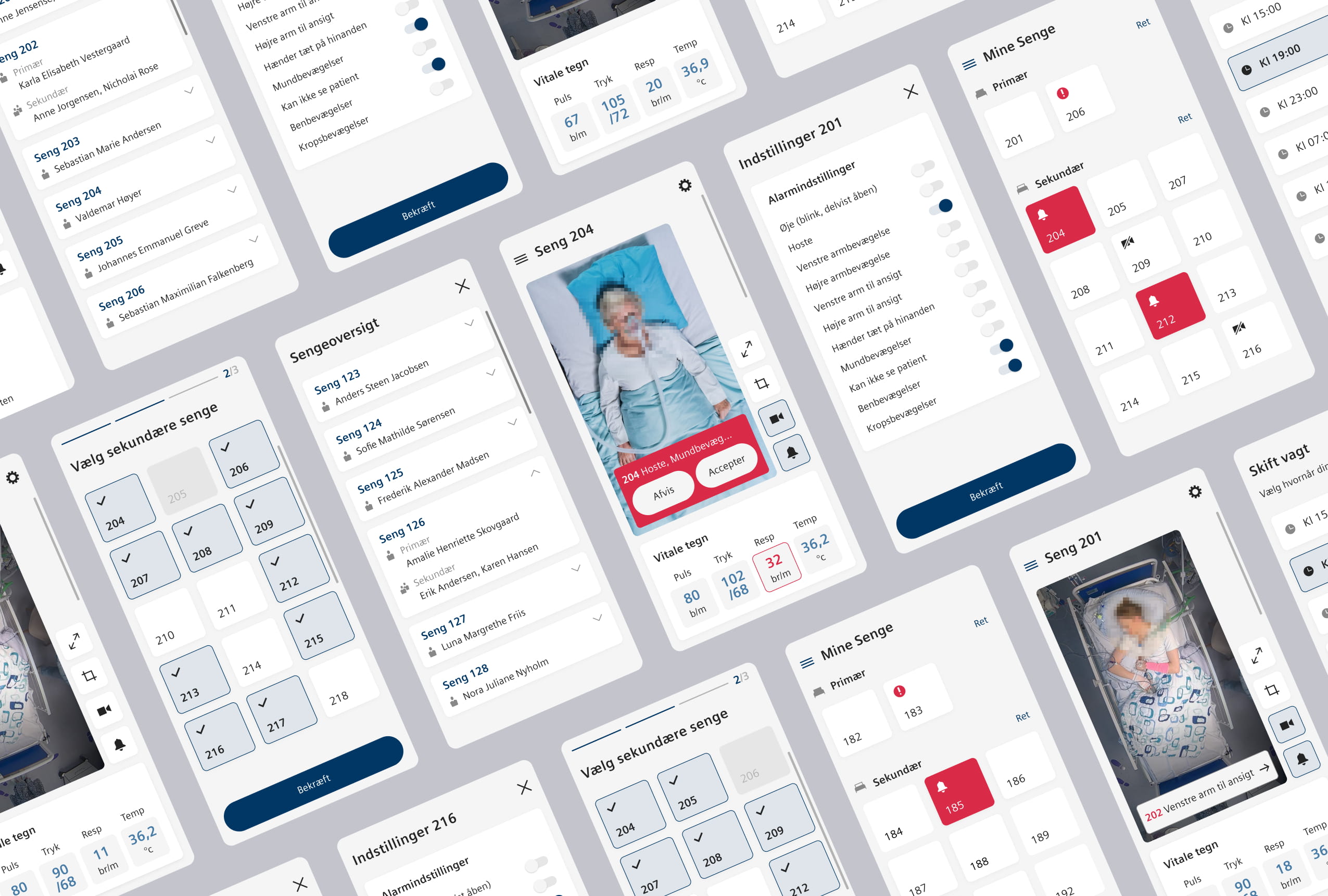
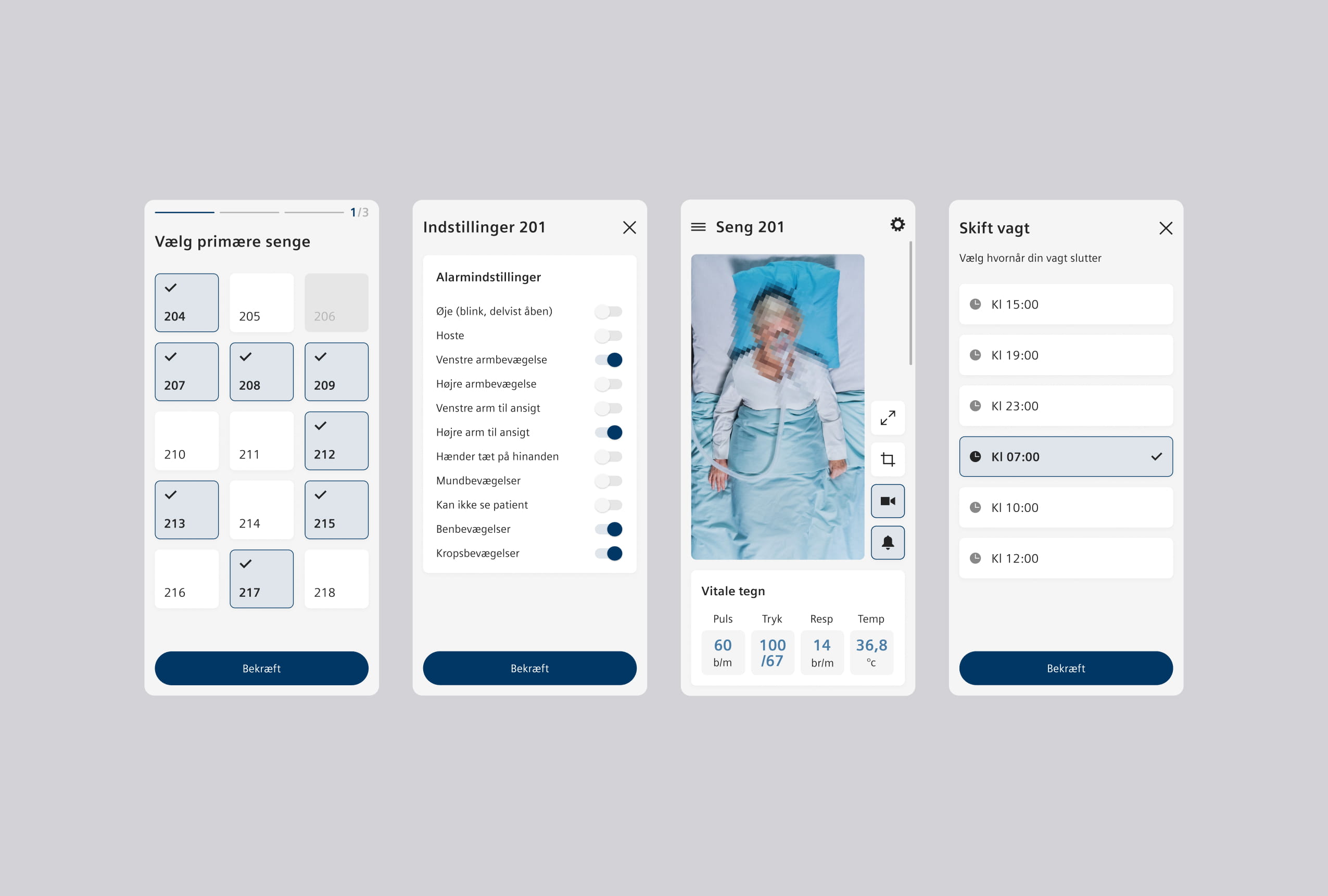
Prototypes, testing and iteration
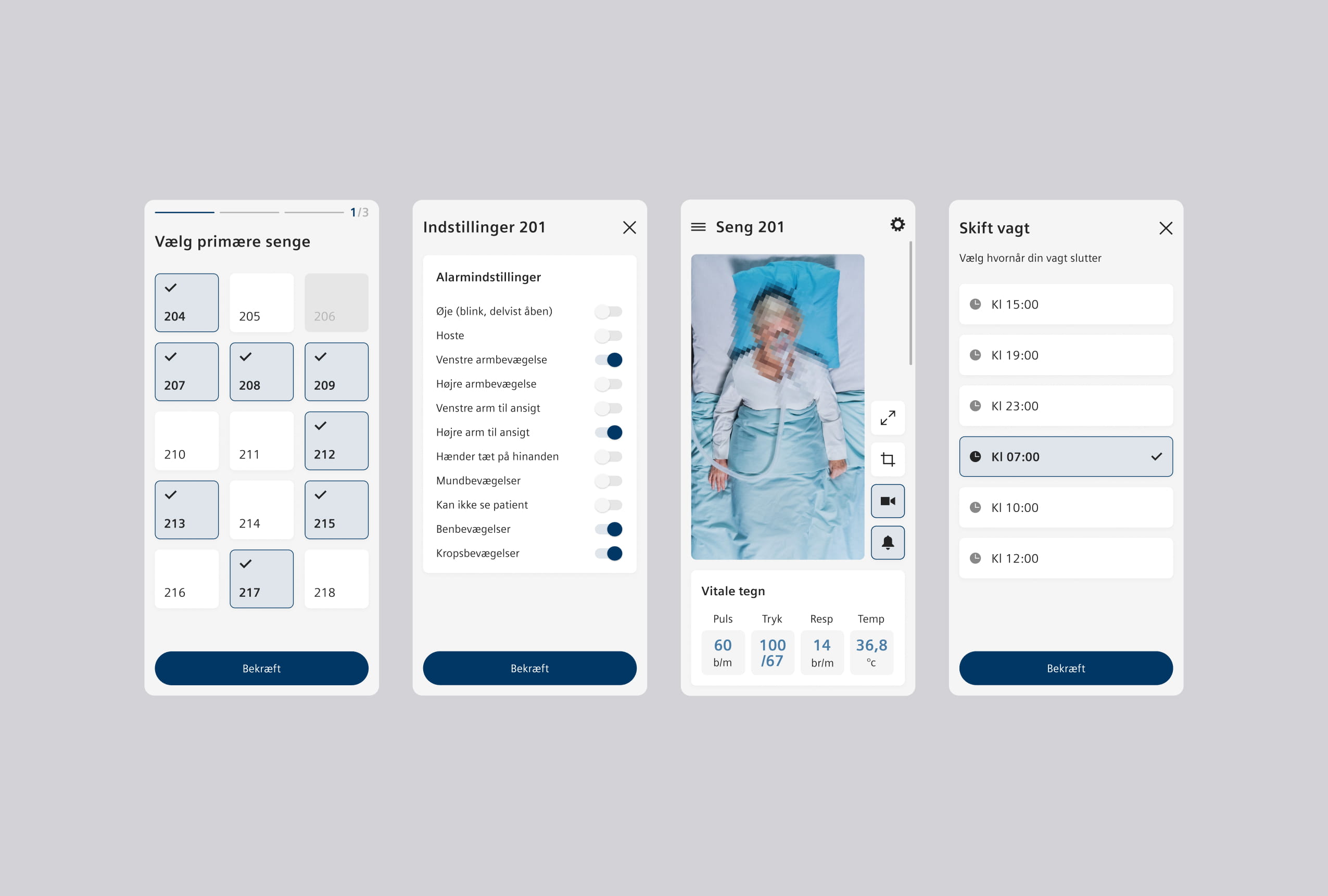
Early concepts were developed into interactive prototypes and tested with ICU staff. Their feedback helped refine the structure, simplify interactions, and prioritize critical information, resulting in an interface clinicians and nurses could rely on in high-pressure situations.
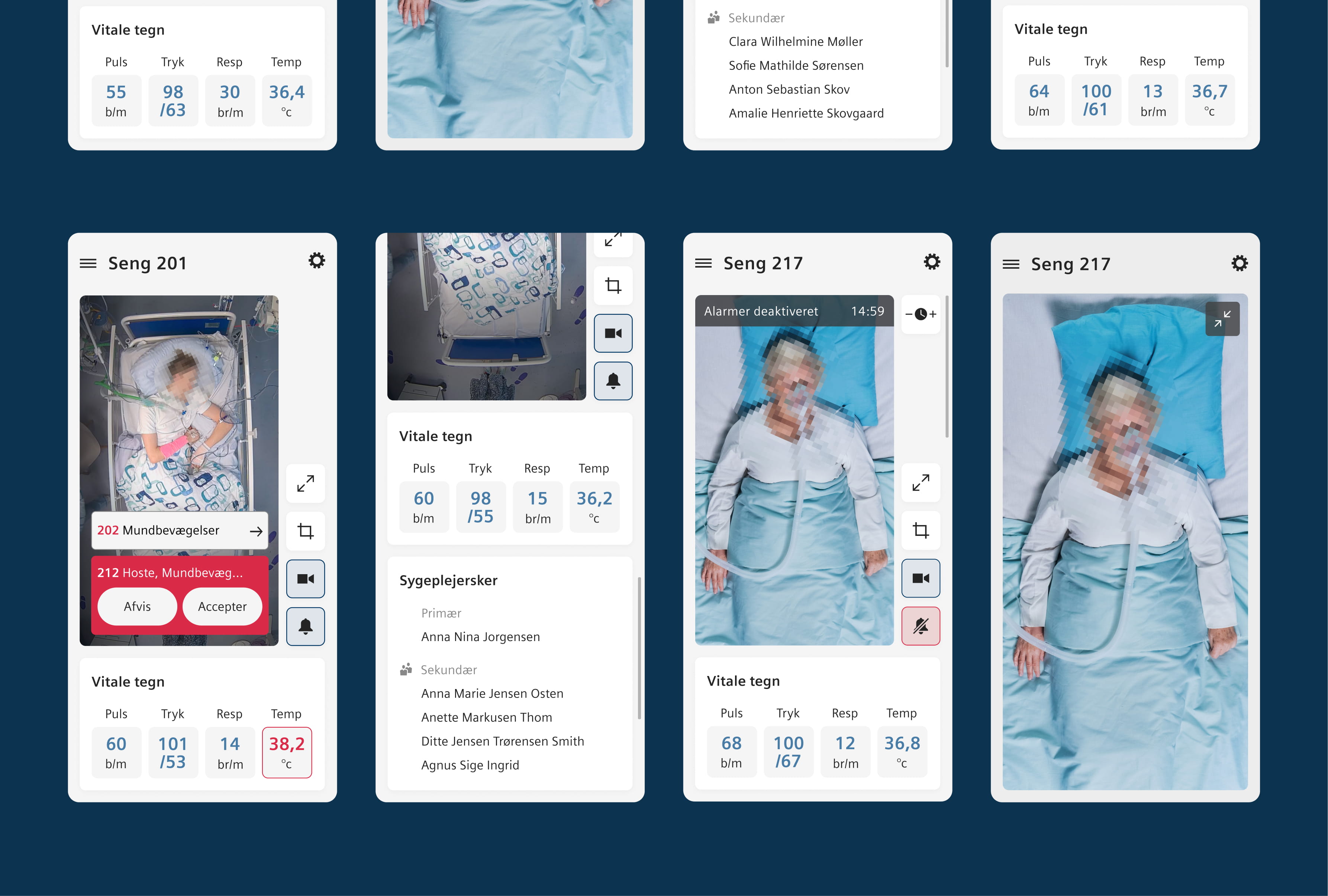
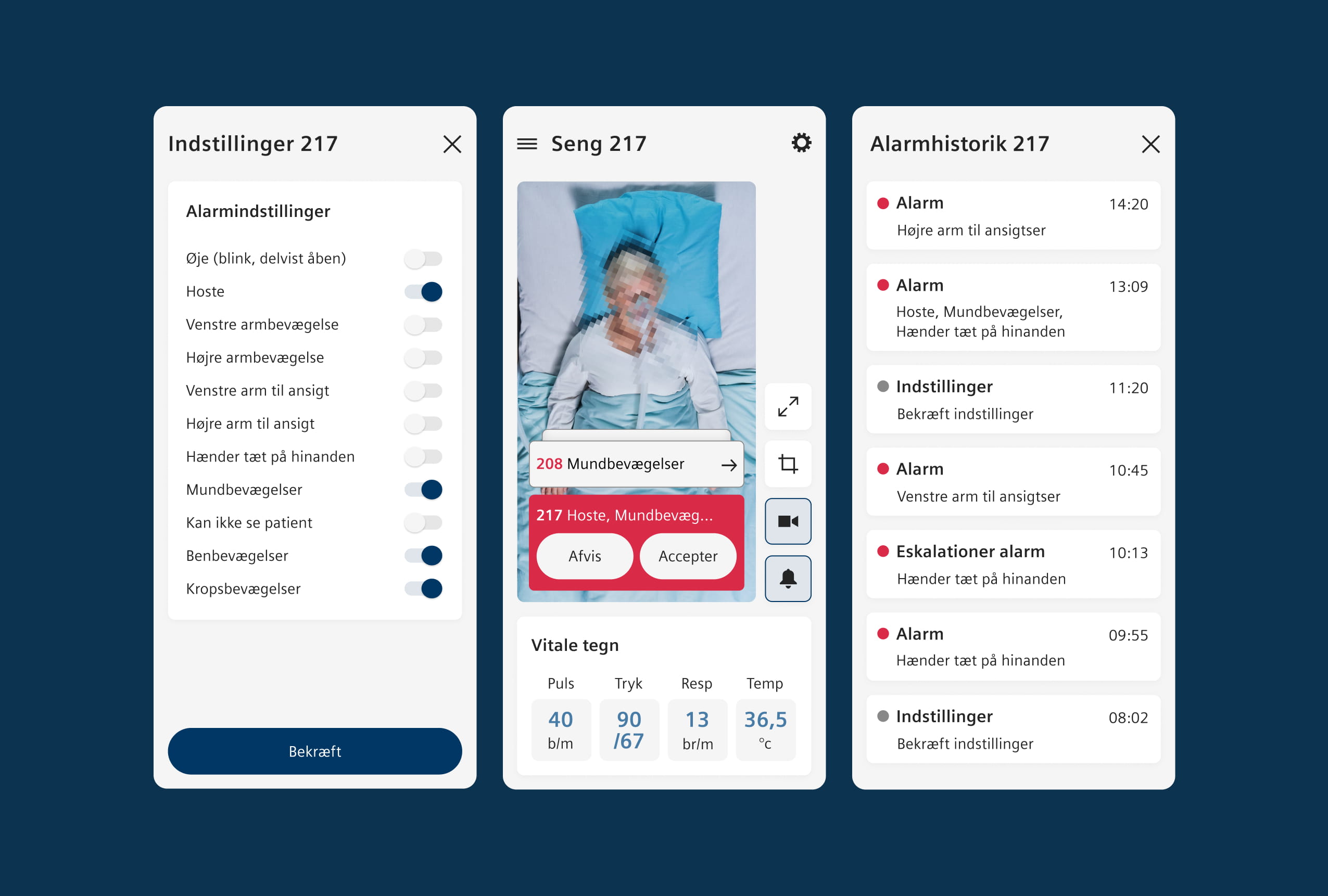
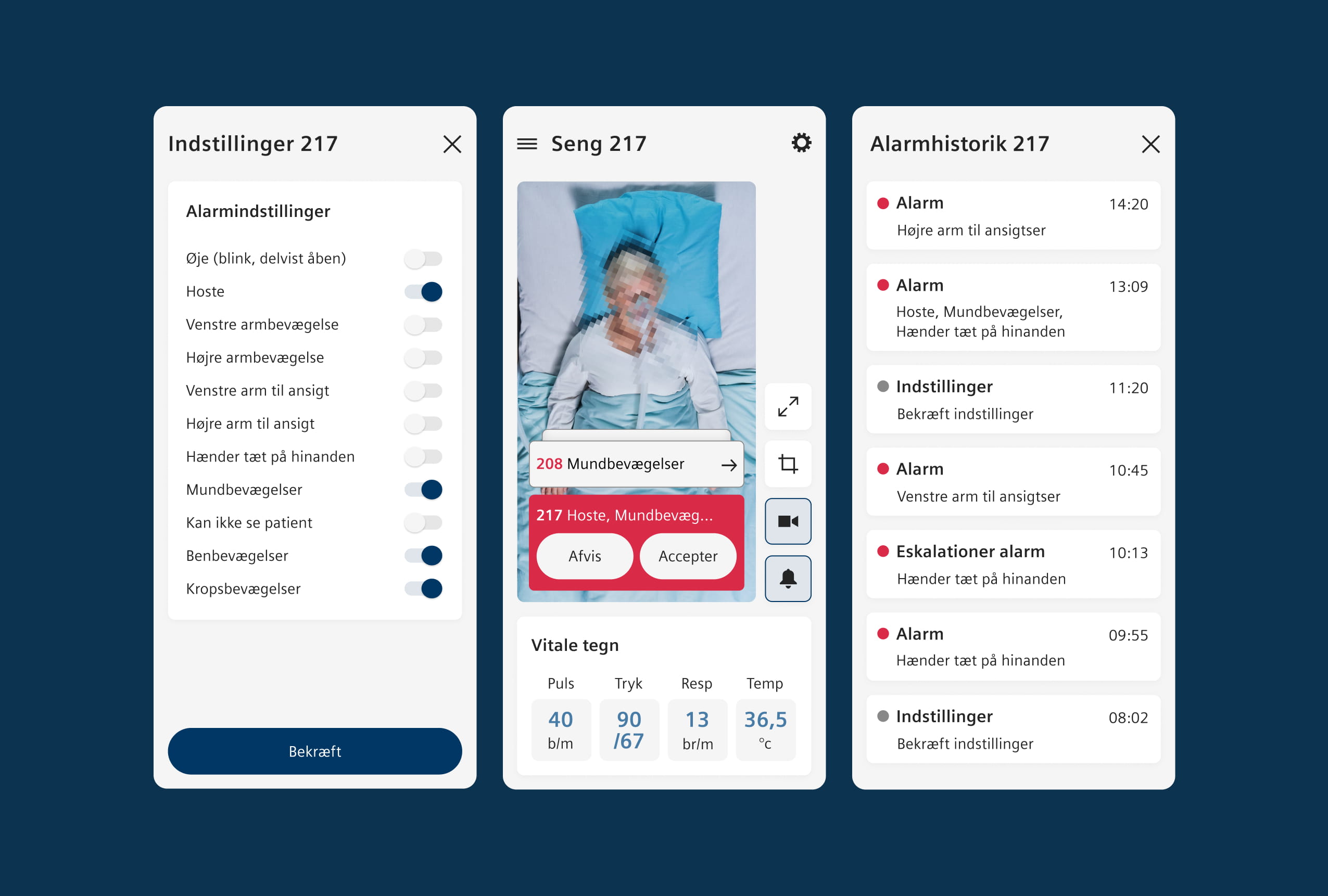
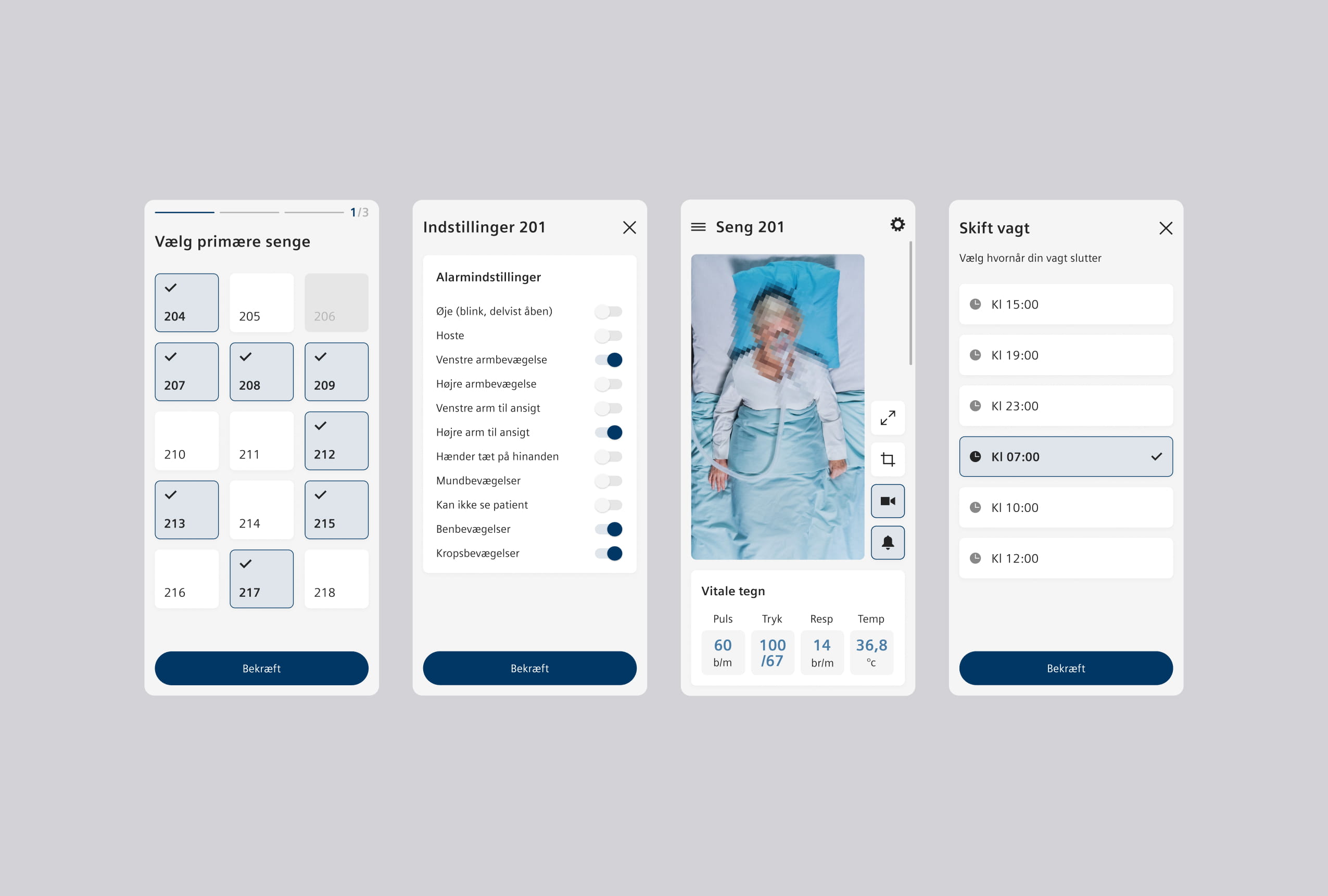
Smart detection and alerts
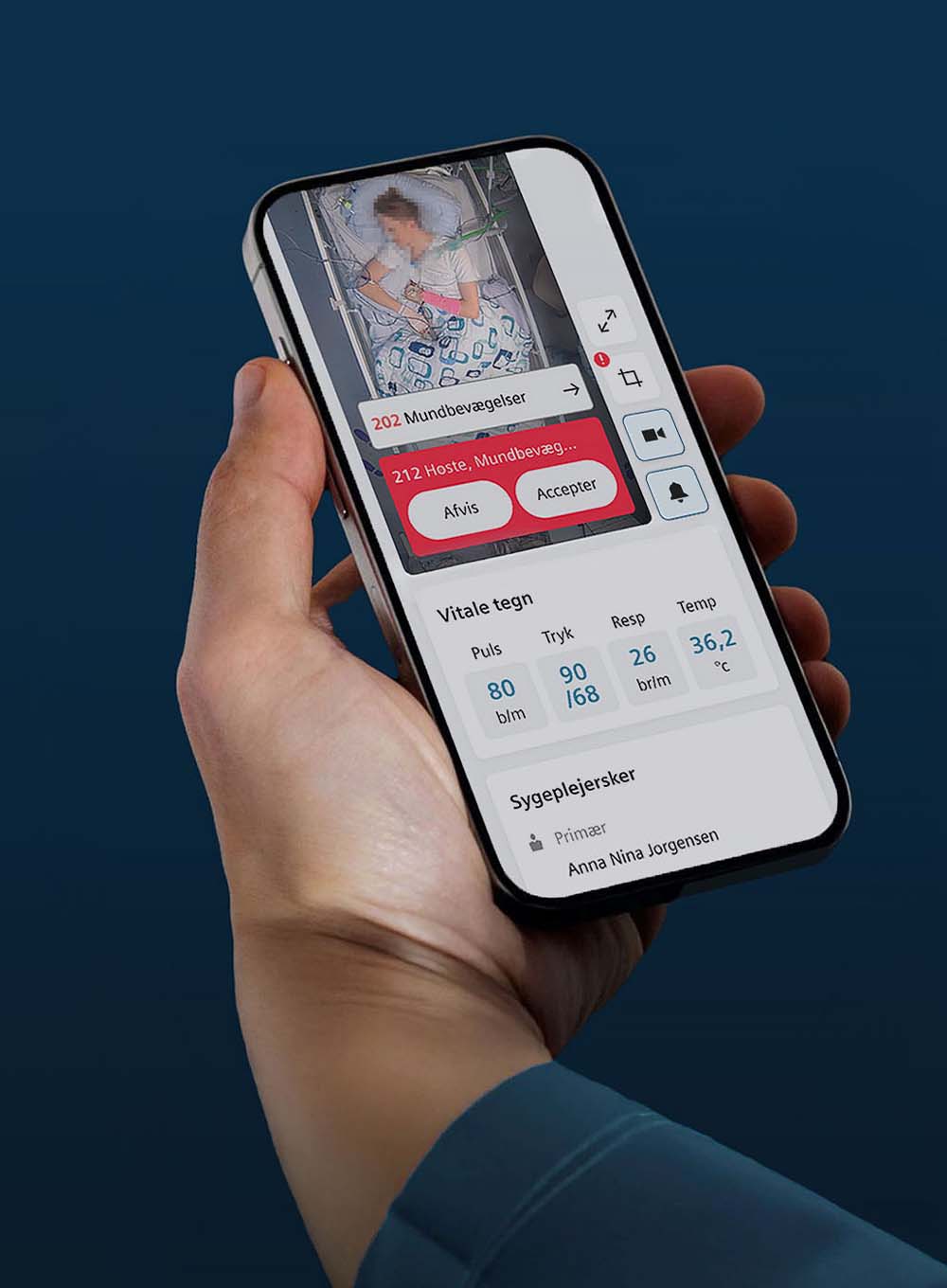
An AI-powered detection system automatically identifies clinically relevant movements such as mouth activity or arm motion, displaying them as alerts. These movements were documented and categorized with staff input to ensure accuracy and relevance.
Nurses can access an overview of all available movements, toggling which ones trigger notifications based on each patient's needs. A complete movement history provides a documented timeline of patient activity, enabling clinicians to track patterns and respond quickly without constant manual observation.
Customised to each patientPattern tracking capabilityEarly movement detection
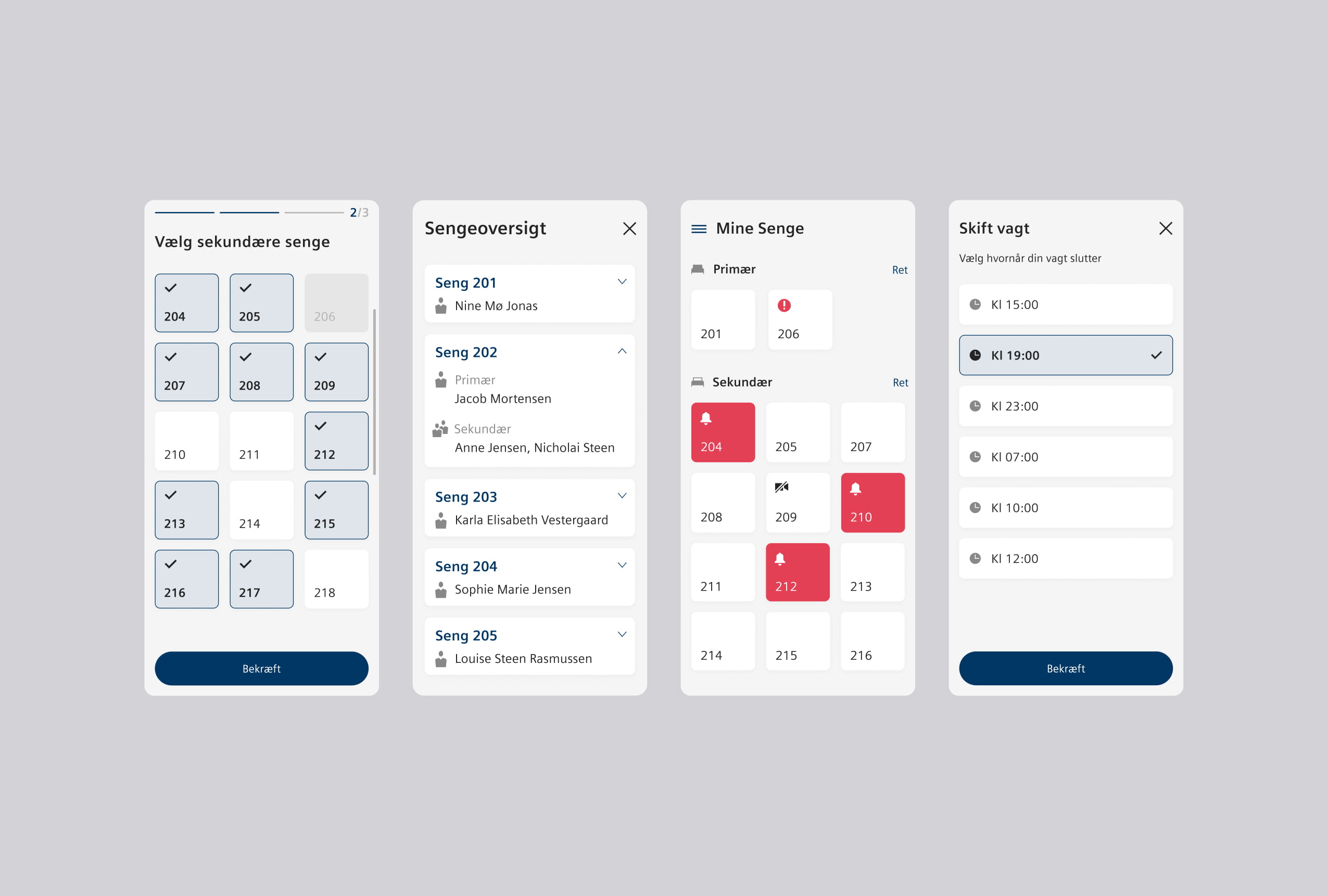
Streamlining workflows
The app streamlined everyday operational tasks. Nurses could assign beds to patients, designate primary and secondary nurses with clear authority over each bed, set up shifts, and extend them when needed. This reduced logistical challenges and made shift planning more efficient.
To make sure every alert was addressed, notifications followed a clear escalation path. If the primary nurse didn’t respond, it was forwarded to the secondary, and if still unanswered, then to all nurses on duty.
Primary nurse → Secondary nurse → All nursesPrimary nurse
↓
Secondary nurse
↓
All nurses
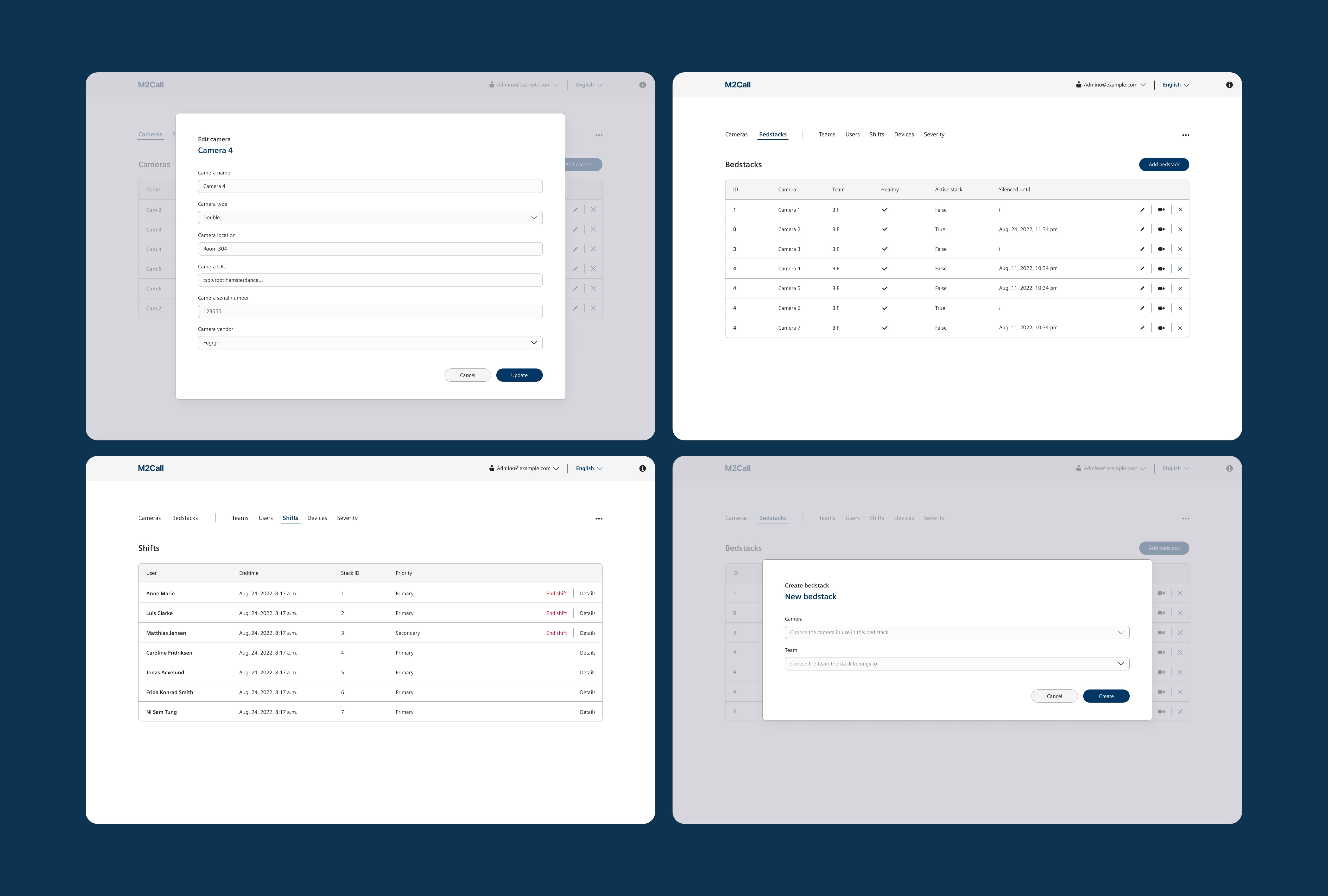
An admin portal gave technicians full control, from camera placement to user management and movement databases. This added security, reduced shift interruptions, and lowered staff workload and stress.
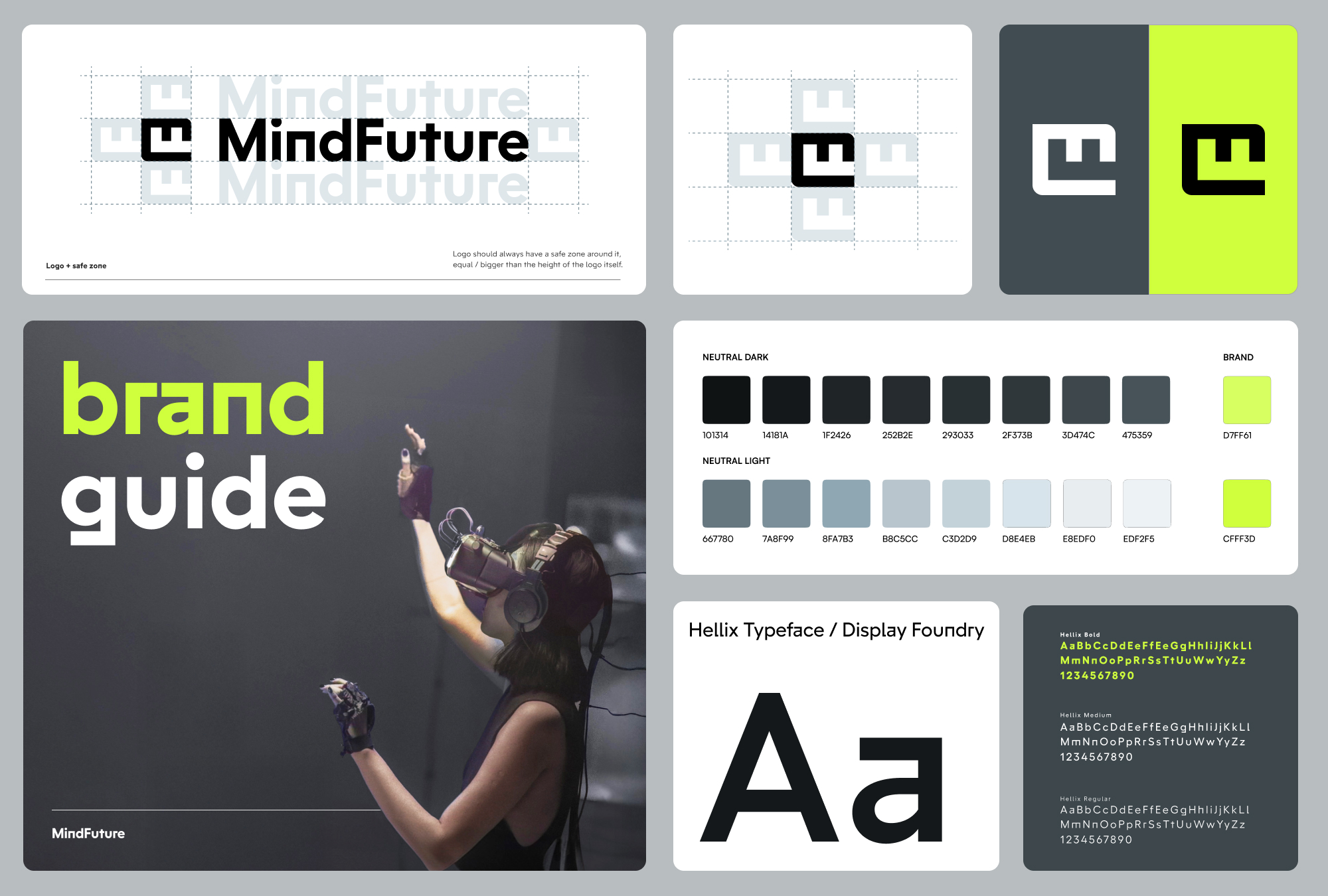
I also built a design system that enabled seamless updates as needs evolved, making it easy to add features, maintain consistency, and deploy improvements without disrupting workflows.